SHREK NEWS
Causes of infection of medical endoscope camera
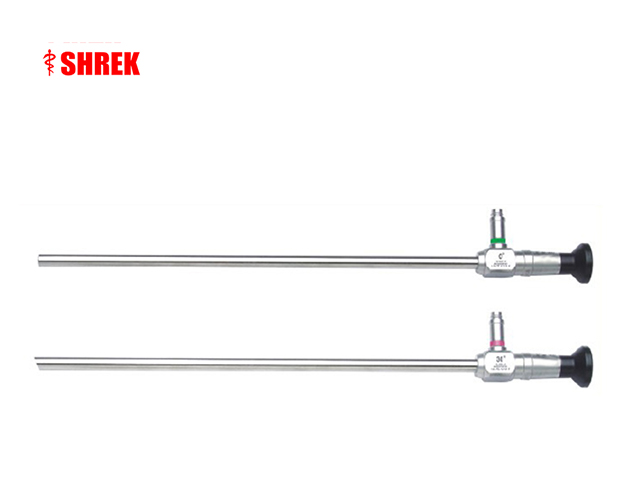
Medical endoscopes are used in a variety of procedures, and if they are not properly cleaned and disinfected, they can become a source of infection for patients. Some of the main causes of infection of medical endoscope camera include:
Inadequate cleaning: If an endoscope is not properly cleaned after use, it can harbor bacteria and other pathogens that can cause infections in subsequent patients. This can occur if the endoscope is not thoroughly brushed and flushed with the appropriate cleaning solution to remove all organic material and debris.
Incomplete disinfection: Even if an endoscope is cleaned properly, it must also be disinfected with an appropriate high-level disinfectant solution to kill any remaining bacteria or other pathogens. If disinfection is not performed correctly, bacteria and other pathogens can survive and cause infections in subsequent patients.
Improper storage: Endoscopes should be stored in a dry, clean environment to prevent contamination. If they are not stored properly, they can become contaminated with bacteria or other pathogens that can cause infections in subsequent patients.
Equipment malfunctions: Endoscope cameras can malfunction or fail, which can lead to the introduction of bacteria or other pathogens into the patient. This can occur if the camera is not properly sterilized or if it is not functioning correctly.
Use on multiple patients: If an endoscope is used on multiple patients without proper cleaning and disinfection between uses, it can spread infections from one patient to another.
To minimize the risk of infection from medical endoscope cameras, it is important to follow established cleaning and disinfection protocols and guidelines, use appropriate disinfectants, store endoscopes properly, and regularly inspect and maintain equipment. Healthcare providers should also be vigilant in monitoring for any signs of infection in patients who have undergone endoscopic procedures.
Endoscopic infection solution
Preventing endoscopic infections requires a multifaceted approach that includes the following strategies:
Cleaning and disinfection: The most important step in preventing endoscopic infections is ensuring that endoscopes are properly cleaned and disinfected. Healthcare facilities should establish and follow strict cleaning and disinfection protocols for endoscopes, and should train staff on proper techniques.
Sterilization: Some endoscopes may require sterilization rather than high-level disinfection to prevent infection. Healthcare facilities should consult the manufacturer's instructions to determine the appropriate sterilization method for each type of endoscope.
Regular maintenance and inspection: Endoscopes should be regularly inspected and maintained to ensure that they are functioning properly and that they are not damaged or contaminated. Healthcare facilities should have a schedule for routine maintenance and inspection, and should train staff on how to identify and report any issues.
Single-use endoscopes: In some cases, single-use endoscopes may be appropriate to reduce the risk of infection. These endoscopes are used once and then discarded, eliminating the need for cleaning and disinfection.
Patient screening: Patients should be screened for infections prior to endoscopic procedures to prevent the spread of infections from one patient to another. Patients with known infections should be treated and/or isolated to prevent transmission.
Environmental hygiene: Healthcare facilities should maintain strict environmental hygiene to prevent the spread of infections. This includes cleaning and disinfecting surfaces and equipment, as well as implementing hand hygiene protocols for staff and visitors.
By implementing these strategies, healthcare facilities can reduce the risk of endoscopic infections and ensure the safety and well-being of their patients.